Antibiotic therapy treatment is a vital tool for infection control, preventing and managing bacterial infections. Its role is significant in community settings and medical procedures like dental work. Effective implementation requires strategic measures such as targeted patient selection, optimized dosage, coordinated care, and educational initiatives. However, antimicrobial resistance (AMR) poses a challenge due to misuse, leading to future strategies focusing on improved infection prevention, responsible prescribing, novel agents, digital monitoring, and prudent antibiotic use in dentistry to combat AMR and preserve treatment options for future generations.
Antibiotic therapy treatment is a powerful tool in the fight against infectious diseases, with a primary goal of preventing the spread of infections. This comprehensive article explores the role of antibiotics in infection control, delving into effective implementation strategies to curb the transmission of pathogens. We examine challenges in current practices and discuss future directions toward safer antibiotic use, emphasizing the importance of understanding antibiotic therapy for optimal public health outcomes.
- Understanding Antibiotic Therapy: The Role in Infection Control
- Strategies for Effective Implementation to Prevent Spread
- Challenges and Future Directions for Safer Antibiotic Use
Understanding Antibiotic Therapy: The Role in Infection Control

Antibiotic therapy treatment plays a pivotal role in infection control, acting as a powerful tool to prevent and combat bacterial infections. It involves the use of antibiotics, substances that inhibit or destroy harmful microorganisms like bacteria. By disrupting the growth and multiplication of these pathogens, antibiotics help to stop the progression of an infection and reduce its impact on the body. This therapy is particularly crucial when dealing with widespread infections, such as those in community settings, where quick intervention can prevent further spread.
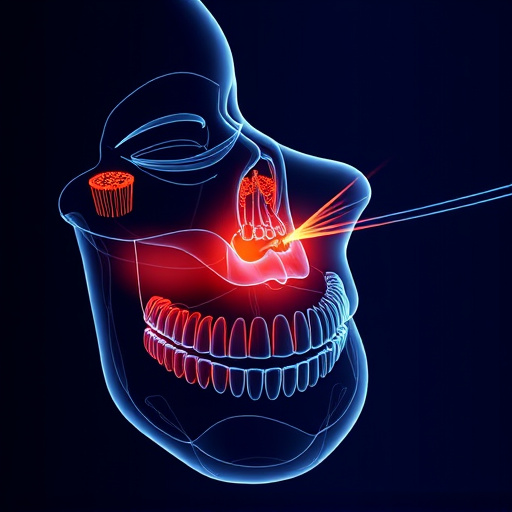
In addition to its direct antimicrobial effects, antibiotic therapy treatment supports other medical procedures, like dental cleanings and tooth repair. In the context of oral health, antibiotics may be prescribed to manage or prevent infections associated with dental procedures, including cosmetic dentistry treatments. This multifaceted approach ensures that infections are controlled not only at the site of infection but also systemically, contributing to overall well-being and minimizing complications from both common and specialized medical interventions.
Strategies for Effective Implementation to Prevent Spread

To implement antibiotic therapy treatment effectively and prevent infection spread, several strategic measures must be taken. Firstly, proper patient selection is crucial; identifying individuals at high risk of infection allows for targeted therapy, maximising its benefits while minimising unnecessary exposure to antibiotics. Additionally, optimisation of dosage regimens ensures that antibiotics are administered optimally, enhancing their efficacy and reducing the likelihood of resistance development.
Co-ordination among healthcare providers is another vital component. Comprehensive communication facilitates a seamless transition from one care setting to another, ensuring continuous antibiotic administration without gaps. Furthermore, integrating educational initiatives for patients and caregivers can foster responsible antibiotic use, promoting awareness about proper hygiene practices and adherence to treatment protocols. This holistic approach, encompassing both medical strategies and patient education, aligns with the goal of preventing infection spread while effectively managing antibiotic therapy treatment.
Challenges and Future Directions for Safer Antibiotic Use

Despite significant advancements in medicine, one of the biggest challenges in antibiotic therapy treatment remains ensuring safe and effective use to prevent infection spread. The growing issue of antimicrobial resistance (AMR) poses a severe threat, rendering once-potent antibiotics less effective over time. This complex problem arises from excessive prescription, inappropriate dosing, and misuse of antibiotics, often driven by patient expectations and limited access to quality healthcare.
Looking ahead, future directions for safer antibiotic use focus on several key areas. These include enhancing infection prevention practices, promoting responsible prescribing guidelines, and developing novel antimicrobial agents. Additionally, integrating digital health technologies can improve monitoring and adherence to treatment protocols. In the context of dental procedures, such as tooth repair or extractions, where antibiotics are frequently prescribed, these strategies become even more crucial. Encouraging children’s dentistry practices that align with prudent antibiotic use could significantly contribute to combating AMR on a broad front, ensuring effective treatments for both common and complex infections well into the future.
Antibiotic therapy treatment plays a pivotal role in infection control, but its effective implementation faces challenges. To prevent further spread of antimicrobial resistance, future strategies should focus on tailored prescription guidelines, patient education, and innovative delivery methods. By balancing access to life-saving antibiotics with responsible use, we can ensure their effectiveness for current and future generations.