Antibiotic therapy treatment involves using medications to fight bacterial infections, with two main types: local and systemic. Local therapy targets specific areas through topical applications or direct delivery, like dental procedures, while systemic therapy circulates throughout the body to treat widespread infections. The choice between these methods depends on infection severity, location, and patient health, aiming to minimize side effects for localized issues and provide broad-spectrum coverage for severe conditions. Proper administration of antibiotic therapy, combining both local and systemic approaches, is crucial for optimal treatment outcomes and addressing growing concerns about antibiotic resistance.
Antibiotic therapy, a cornerstone of modern medicine, offers local or systemic treatments to combat bacterial infections. Understanding these distinct approaches is vital for optimal patient care. This article delves into the mechanisms and applications of each strategy, highlighting when local or systemic antibiotics are indicated. We explore effective administration techniques to ensure antibiotic therapy treatment success while minimising resistance. By understanding these nuances, healthcare professionals can navigate the complex world of antibiotic prescription for better patient outcomes.
- Understanding Antibiotic Therapy: Types and Mechanisms
- Local vs Systemic Treatment: When and Why It Matters
- Effective Administration: Strategies for Optimal Antibiotic Therapy
Understanding Antibiotic Therapy: Types and Mechanisms

Antibiotic therapy treatment involves the use of medications to combat bacterial infections. The primary goal is to eliminate harmful bacteria while promoting the recovery of healthy cells. Antibiotics work by interfering with specific processes essential for bacterial growth and survival, such as disrupting their cell walls, inhibiting protein synthesis, or interfering with vital metabolic pathways. These mechanisms ensure that antibiotics target and destroy bacteria without causing harm to the host cells.
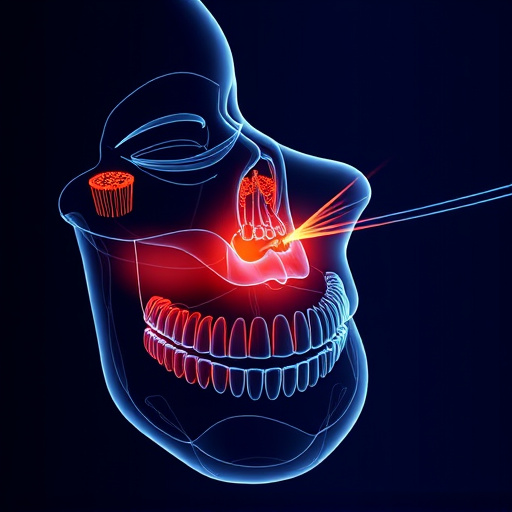
There are two primary types of antibiotic therapy: local and systemic. Local antibiotic therapy focuses on treating infections in specific areas, often through topical applications or direct delivery to the affected site. This approach is common in dental procedures where infections might arise from tooth extractions or other oral surgeries. Systemic antibiotic therapy, on the other hand, involves administering antibiotics through oral or intravenous routes, allowing them to circulate throughout the body and target systemic infections. While general dentistry practices often prescribe local antibiotics for minor issues like dental fillings or surface infections, more severe conditions, such as those requiring dental implants, might necessitate systemic treatment to ensure comprehensive bacterial eradication.
Local vs Systemic Treatment: When and Why It Matters

In the realm of antibiotic therapy treatment, understanding the distinction between local and systemic approaches is paramount for effective healthcare. Local treatment involves directly administering antibiotics to the affected area, focusing on a specific infection site. This method is often employed for localized infections like dental abscesses or skin wounds, where topical or oral antibiotics can sufficiently combat the pathogens without disrupting the body’s overall balance. On the other hand, systemic treatment requires introducing antibiotics into the bloodstream, allowing them to circulate and target infections throughout the body. Such an approach is indicative of more severe conditions, such as blood infections or widespread bacterial infestations, where quick diffusion and broad-spectrum coverage are essential.
The choice between local and systemic antibiotic therapy treatment depends on various factors, including infection severity, location, and patient health status. For instance, comprehensive dental care often incorporates local treatments for tooth repair and gum infections to minimize side effects and promote faster healing. In contrast, systemic antibiotics might be necessary for treating a patient’s overall immune system response to a bacterial invasion, ensuring a more holistic recovery. Recognizing when each approach is warranted ensures optimal outcomes and minimizes the potential for antibiotic resistance, a growing concern in modern healthcare.
Effective Administration: Strategies for Optimal Antibiotic Therapy

Effective administration is key to ensuring optimal antibiotic therapy treatment outcomes. Healthcare providers must consider both local and systemic approaches to manage infections appropriately. Localized treatments, such as targeted topical antibiotics or dental crowns in cases of oral infections, can be highly effective by directly addressing the affected area. This strategy is particularly relevant in preventive dentistry, where regular dental cleanings play a crucial role in reducing the risk of localized bacterial infections.
For systemic infections, oral administration of antibiotics is common. Strategizing the timing and duration of medication intake is vital to enhance absorption and minimize side effects. Additionally, combining topical and systemic approaches can be beneficial for certain conditions. This integrated approach ensures comprehensive coverage while avoiding potential challenges associated with single-site treatments, making it a robust strategy in managing antibiotic therapy.
Antibiotic therapy treatment, whether local or systemic, plays a pivotal role in combating infections. Understanding the nuances of different mechanisms and administering them effectively is key to optimal patient outcomes. By tailoring antibiotic therapy to specific needs, healthcare professionals can ensure successful infection management while mitigating resistance risks. Local vs. systemic approaches each have their merits, and knowing when to apply each strategy is essential for effective antibiotic therapy treatment.