Shockwave therapy for pain is a popular, non-invasive option for muscular and joint issues, but insurance coverage varies. To access this treatment, individuals should understand their policy, consult with both their insurer and healthcare provider, and obtain pre-authorization. This process ensures coverage for conditions like chronic post-injury pain, avoiding unexpected out-of-pocket expenses, and facilitating effective pain management through shockwave therapy.
Is shockwave therapy for pain covered by insurance? This comprehensive guide explores the financial aspects of non-invasive treatment for various conditions. We break down how and why shockwave therapy is increasingly recognized, its impact on patient outcomes, and the key factors influencing insurance reimbursement policies. Learn essential tips for navigating claims processes, ensuring access to this potentially life-changing treatment.
- Understanding Shockwave Therapy for Pain Coverage
- Factors Influencing Insurance Reimbursement
- Navigating the Process: Tips for Patients
Understanding Shockwave Therapy for Pain Coverage

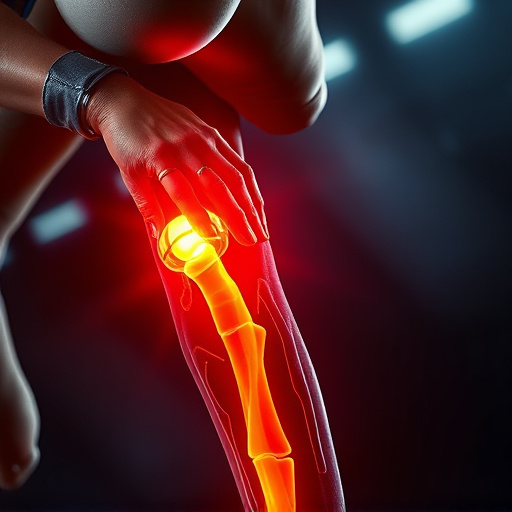
Shockwave therapy for pain has gained popularity as a non-invasive treatment option for various muscular and joint conditions. However, when considering this therapy, understanding insurance coverage is essential. Many health insurance plans do offer coverage for shockwave therapy under specific circumstances. Typically, if your condition meets the criteria for conservative or alternative treatments, your insurance provider might approve the procedure. This often includes cases where traditional therapeutic exercises and physical therapy haven’t provided sufficient relief.
Before pursuing shockwave therapy, it’s crucial to communicate with both your healthcare provider and insurance company. They can guide you on what conditions are typically covered, the process for seeking pre-authorization, and any out-of-pocket expenses you might incur. Additionally, staying informed about your policy’s terms and conditions related to alternative treatments will ensure a smoother journey towards managing your pain effectively through shockwave therapy.
Factors Influencing Insurance Reimbursement

Several factors can influence whether insurance covers shockwave therapy for pain, a non-invasive treatment gaining popularity in wellness care and injury rehabilitation. Firstly, the specific plan details play a crucial role; certain policies may not cover alternative treatments, or they might have caps on out-of-pocket expenses. Secondly, diagnostic criteria are essential; if a healthcare provider recommends shockwave therapy as a valid treatment for a covered condition, such as chronic pain resulting from post-injury care, the chances of reimbursement increase. Additionally, geographical location can impact insurance coverage due to varying healthcare regulations and policies across regions.
Understanding your insurance policy and consulting with both your insurer and healthcare provider is vital to navigating these factors. The provider should be able to guide you through the process, ensuring that shockwave therapy for pain is considered within the scope of your wellness care plan, especially when used as a part of comprehensive post-injury care or injury rehabilitation strategies.
Navigating the Process: Tips for Patients
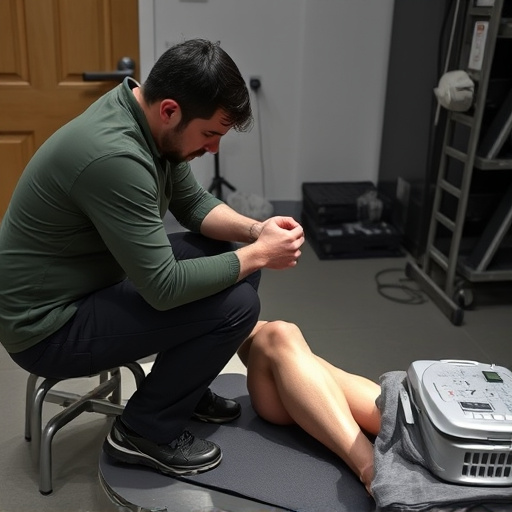
Navigating the process of shockwave therapy for pain coverage by insurance can be a bit daunting, but understanding your options and rights as a patient is essential. The first step is to review your policy thoroughly. Many insurance plans now include coverage for non-invasive treatments like shockwave therapy for soft tissue injuries, especially when prescribed by a qualified healthcare provider. Check your policy’s in-network and out-of-network provisions, as well as the specific terms related to physical therapy, chiropractic care, or specialized pain management services.
Once you’ve confirmed coverage, contact your insurance carrier directly to obtain pre-authorization for your treatment. This step ensures that your healthcare provider can bill your insurance appropriately and helps avoid unexpected out-of-pocket expenses. Keep records of all communication, including emails, letters, and any documents related to your shockwave therapy plan. These will be useful if you encounter any issues or need to appeal a decision regarding coverage.
Shockwave therapy for pain has gained recognition as an effective treatment option, and understanding its insurance coverage can significantly impact patient access. While reimbursement policies vary across different insurance providers, many are now recognizing the benefits of this non-invasive approach. By navigating the process with knowledge and patience, patients can increase their chances of obtaining coverage for shockwave therapy, making it a viable choice for managing chronic pain.